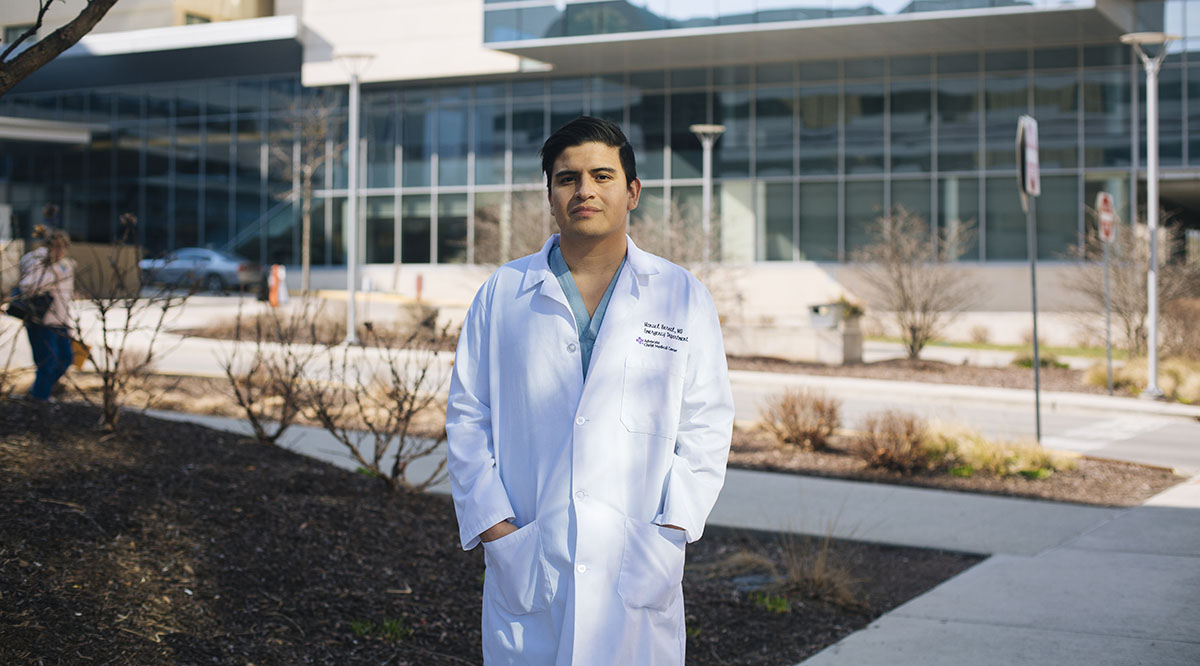
When the COVID-19 pandemic began to hit the Chicago area earlier this spring, Manuel Bernal, MD, was anxious to start treating the sick patients who would come into the emergency department at Advocate Christ Medical Center in Oak Lawn, Illinois.
He worried about adjusting to the additional time and effort required to don the appropriate protective gear while juggling nearly a dozen patients at once and the extra precautions he would have to take to avoid bringing the virus home to his loved ones. But he was also eager to do what he felt was his calling.
In fact, for Bernal, a second-year emergency medicine resident, the frenzy of working long shifts in the emergency department has been a welcome distraction from another point of anxiety that he confronts every day: the fear that his work permit could be revoked and he could be deported to Mexico, a country he hasn’t set foot in since he was 2 years old.
Bernal is one of an estimated 200 medical students and residents who have been able to pursue careers in medicine because of the Deferred Action for Childhood Arrivals (DACA) program, which President Barack Obama put in place in 2012 to provide some protections to undocumented immigrants who came to the United States as children. DACA recipients are authorized to work in the United States.
“The idea of [DACA] being revoked or ended is kind of terrifying, especially with this current pandemic. It is frustrating that I could be needed by my country so much, but not enough to be wanted.”
Manuel Bernal, MD
Second-year emergency medicine resident at Advocate Christ Medical Center
The Trump administration moved to rescind DACA in 2017 — a decision that the U.S. Supreme Court vacated on June 18, ruling that the Department of Homeland Security did not follow the legally required process. An amicus brief filed by the AAMC on behalf of dozens of health professional education groups supported claims that the federal government terminated DACA without adequately considering the negative consequences of rescinding a long-standing policy. The brief noted that ending the program would leave a hole in the U.S. health care workforce that would be difficult to fill and would disadvantage medical schools and teaching hospitals that have invested in DACA recipients who are training at U.S. institutions.
The Supreme Court’s decision grants DACA recipients a temporary reprieve from the fear of immediate revocation of the program, but it leaves open the ability of the federal government to end the program by providing a more thorough justification.
DACA has taken on new meaning in the past few months during a pandemic that has strained hospitals and required health care workers — about 29,000 of whom are DACA recipients, according to the Center for American Progress — to put themselves at risk of infection in order to prevent spread and treat patients.
“The idea of [DACA] being revoked or ended is kind of terrifying, especially with this current pandemic,” Bernal says. “It is frustrating that I could be needed by my country so much, but not enough to be wanted.”
Immigration advocates and health professions organizations, including the AAMC, have lobbied for legislation that would give DACA recipients more permanent legal status, but bills, such as the American Dream and Promise Act, have stalled in Congress.
Bringing much-needed diversity to the workforce
In the brief filed with the Supreme Court last fall, the AAMC urged the justices to consider the negative consequences that would result from rescinding DACA. Not only would it damage the career prospects of thousands of young professionals, the brief argued, but it would nullify an estimated $5 million worth of financial investment that U.S. medical schools and hospitals have spent to train DACA recipients as of February 2019 and would cost the United States highly skilled medical professionals at a time when the country is facing a physician shortage.
By 2032, the United States will have an estimated 46,900 to 121,900 fewer physicians than it needs as the country’s population ages and older doctors retire — a shortfall that disproportionately impacts poor, underserved, and rural areas, according to the brief.
In addition to increasing the numbers of trained physicians in the country, DACA recipients tend to bring much-needed diversity and resilience to the profession, says Mark Kuczewski, PhD, director of the Neiswanger Institute for Bioethics and Healthcare Leadership at Loyola University Chicago Stritch School of Medicine, the first U.S. medical school to accept DACA recipients.
“We have a huge diversity problem in medicine,” Kuczewski says. “We’re not turning out a workforce that’s really appropriate to serve the community. There’s a shortage of people who look like the community and understand underserved communities.”
Kuczewski believes broader representation in medicine is even more important during the pandemic. That’s in part because immigrant and minority populations need to feel comfortable seeking testing and treatment, which are central to protecting not only those communities but also public health overall.
Serving the underserved

For Denisse Rojas, a fourth-year medical student at Icahn School of Medicine at Mount Sinai in New York City, it was the desire to serve undocumented immigrants like her own family that inspired her to pursue a career in emergency medicine and a master’s degree in public policy from the John F. Kennedy School of Government at Harvard University.
Rojas, a DACA recipient who was brought to the United States from Mexico as an infant, remembers the struggles of growing up without insurance and relying on free clinics and emergency departments for health care.
“People are vulnerable and scared,” she says. “I am able to relate to people in those situations.”
Although Rojas is still a student and hasn’t directly treated COVID-19 patients, she volunteers with her institution’s student-run free clinic, the East Harlem Health Outreach Partnership, which serves many Spanish-speaking, undocumented immigrants.
“It feels like I’ve been waiting for an eternity to have stability.”
Denisse Rojas
Fourth-year medical student at Icahn School of Medicine at Mount Sinai
Since the pandemic hit, Rojas and the other volunteers have switched to telehealth checkups, personally calling patients who were discharged from the hospital after battling COVID-19. They have also begun delivering food and prescriptions, and they have raised over $60,000 to help undocumented immigrants who have been hit by economic hardship and were not eligible for federal stimulus funds.
“People need help now more than ever,” Rojas says. “There’s a disproportionate impact to people of color.”
While Rojas is juggling her studies, volunteering, and advocacy, she has also had to deal with the stress of living far away from her relatives, concerns over health problems in her family, and the impending Supreme Court decision on DACA.
“For me, DACA has been such a blessing,” she says.
But, in an interview before the Supreme Court's decision was announced, Rojas said the uncertainty of her future weighs on her as she tries to plan her fourth-year schedule with the fear that she may not be able to go on to residency.
“It feels like I’ve been waiting for an eternity to have stability,” she says.
Fighting to practice

Since early March, when the reports of COVID-19 patients overwhelming hospitals in New York City were flooding the news, Jirayut New Latthivongskorn, MD, has had little time to think about anything besides his patients and the pandemic.
As a first-year medical resident at Zuckerberg San Francisco General Hospital and Trauma Center, Latthivongskorn regularly works 80-hour weeks. Although San Francisco did not see the same overwhelming numbers of COVID-19 patients as New York, he and his colleagues spent significant time and energy over the past couple of months preparing for a possible surge, counting personal protective equipment supplies, and coming up with contingency plans.
At first, he didn’t worry too much about his own health, since reports suggested that the virus was most dangerous to older and medically vulnerable people, but more stories of healthy, young people becoming ill made the risks feel more like reality.
“Certainly, the COVID-19 pandemic has taken up a huge chunk of my mental space,” Latthivongskorn says. “Anyone could get unlucky, and yet we are in a profession where we are walking directly toward the fire.”
Latthivongskorn, a DACA recipient who came to the United States from Thailand when he was 9, allowed himself little time this spring to think about the impending Supreme Court decision until this month. As one of the plaintiffs on the lawsuit challenging the federal government’s decision to rescind DACA, he began to anticipate the court’s ruling.
“It shouldn’t take a pandemic to show the government, the Trump administration, and the Supreme Court justices what DACA recipients and our families do and why we deserve to continue to be here and to live as Americans. But if it does, I hope that’s one of the possible silver linings.”
Jirayut New Latthivongskorn, MD
First-year resident in family and community medicine at Zuckerberg San Francisco General Hospital and Trauma Center
Over the past few weeks, on Sunday and Wednesday nights, group texts he shares with friends and fellow DACA recipients were filled with concern.
Latthivongskorn said he found comfort in knowing that he’s fought as hard as he could to prove that he — and thousands of other immigrants — deserve to stay in the country.
“It shouldn’t take a pandemic to show the government, the Trump administration, and the Supreme Court justices what DACA recipients and our families do and why we deserve to continue to be here and to live as Americans,” he said in an interview before the decision was announced. “But if it does, I hope that’s one of the possible silver linings.”
Forging ahead in spite of uncertainty

For Diana Andino, MD, a second-year neurology resident at Loyola University Medical Center in Maywood, Illinois, COVID-19 is often most painful when she serves as the main source of communication to her patients’ family members.
Andino, a DACA recipient who immigrated to the United States from Ecuador when she was 11, sees COVID-19 patients only when they have serious complications, such as a stroke or major bleeding. Because of the danger of transmission, family members can’t visit their sick relatives, so Andino must have difficult, life-and-death conversations from afar.
The virus’s elusive nature was also a point of concern for Andino. From the beginning of the pandemic, she and her team have been focused on researching how the virus impacts the nervous system. What started out as anxiety about an unknown virus has become Andino’s new normal, she says.
But she’s also used to living with uncertainty. As an undocumented immigrant, she’s long had to spend her days not knowing whether she’ll be able to continue to work and live in the United States.
“It’s very difficult because I’m away from home and not seeing my family,” Andino says. “While I have the privilege of getting to take care of patients, it was stressful not knowing if I or my colleagues were going to become a patient as well.”
Yet, despite the worry that weighs on DACA medical students and residents while live with uncertainty about the long-term fate of their work permits, many continue to excel in their studies and clinical work — a phenomenon that makes them especially valuable as health care providers, Kuczewski says.
He says that working with the 24 DACA recipients who have graduated from Stritch over the past few years has demonstrated to him their exceptional work ethic, resilience, and ability to push forward through the challenges of medical school despite personal struggles.
“Think about [intensive care units] right now with COVID patients staying three weeks,” Kuczewski says. “The doctor just has to stay focused and keep grinding it out. These young people have those qualities. That’s exactly who you want in medicine.”
