From the world’s first face and eye transplant to a brain implant that allowed a man to speak for the first time in years, breakthroughs in academic medicine are improving scientific understanding and enhancing patients’ lives.
Read about several recent significant advances below.
A breakthrough heart surgery changes lives

Margaret Van Bruggen, left, and Kensley Frizzell, center, received valves from heart transplant recipient Journi Kelly, right, in a “domino” surgery — and the world’s first living mitral valve replacement — at Duke Health in February.
Courtesy Duke Health
Margaret Van Bruggen, 14, was suddenly terribly ill. In November, the high school freshman and cross-country runner from Charlotte, North Carolina, developed a fever, and one morning she collapsed inexplicably.
The cause turned out to be serious: endocarditis, a heart inflammation triggered by a bacterial infection. It had already damaged her mitral valve beyond repair, and she would need a new one.
Usually, surgeons have two replacement options, a bioprosthetic valve made from preserved animal tissue or a mechanical valve made from metal or a similar material. Both types have major drawbacks, including the need to replace the valve as the youngster grows.
“It’s not inconceivable to need several replacement surgeries even at a young age,” says Joseph Turek, MD, PhD, a pediatric heart transplant surgeon at Duke Health in Durham. “Every one of those additional operations carries a higher and higher risk.”
So, in a breakthrough procedure, Turek and his colleague Douglas Overbey, MD, MPH, crafted a third option: using a human donor’s living mitral valve they hoped would grow with the patient.
What unfolded next was a “domino” surgery in which an 11-year-old girl who received a full heart transplant, Journi Kelly, donated her healthy valves to Margaret and to another young patient whose aortic valve had begun to fail.
Margaret’s surgery — the world’s first living mitral valve replacement — was quite complicated, says Turek.
“The location of the mitral valve makes the transplant very difficult technically,” and its complex shape adds to the challenge, he explains. “Also, the mitral valve is extremely important because it connects to the left ventricle, which is responsible for pumping blood to the entire body.”
Still, Turek was confident that the surgery would work.
For one, the team practiced extensively on animals before proceeding. From this work, they also saw that the living valve did grow over time as they’d hoped. “There is no way we would ever do this kind of operation in a child if we weren’t confident it would work,” he says.
In fact, on the day of the surgery, the valve began functioning “perfectly” right on the operating table, Turek reports.
“It was a great moment,” he says. “You start out [years earlier] with this idea that maybe you can change lives, and then you see it come to fruition. That’s a peak experience. And then you think about the thousands more kids who could be helped in the future.”
For the families involved, the surgeries certainly were peak moments as well.
“When they asked us if we wanted to donate the healthy parts of Journi’s heart, I said, ‘Where do we sign?’” says Journi’s stepmother, Rachel Kinsey.
After the surgery, Margaret wrote Journi a thank-you letter, adds Enam Kinsey, Journi’s mother. It read: “You gave me a part of your old heart … guess what you are? Amazing. That’s what you are.”
The power to speak
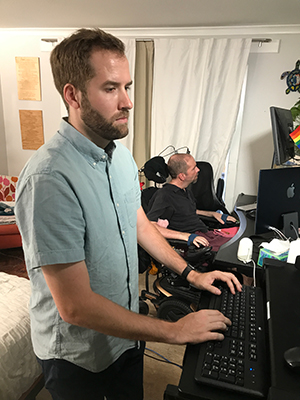
Bioengineer Nicholas Card, PhD, above, a fellow at the UC Davis Neuroprosthetics Lab, prepares the device that allows Casey Harrell, in the background, to speak.
Courtesy UC Davis Health
At age 45, Casey Harrell could no longer eat or dress by himself, and he needed a motorized wheelchair to navigate his Oakland, California, home. But what probably pained him most since developing amyotrophic lateral sclerosis (ALS) was losing his ability to speak.
Now, following surgery at UC Davis Health, Harrell can utter “I love you” — and far more — to his wife and daughter with the help of experimental technology and a sophisticated artificial intelligence (AI) program.
The system he uses — a type of brain-computer interface (BCI) — is quite complex.
Four electrode arrays implanted in Harrell’s brain pick up the nerve impulses that fire when he tries to move his mouth, tongue, and jaw to formulate sounds. Then, cables secured to his head send those impulses to computers that have the ability to translate them into units of human speech.
Simply put, the device sidesteps Harrell’s impaired facial muscles and instead relies on the part of his brain that first lays down the instructions for speech.
“People who have trouble communicating often feel lonely and isolated,” says UC Davis neurosurgeon David Brandman, MD, PhD. “Other options exist, such as devices that use a person’s gaze to select phrases, but those can be cumbersome to use. Our system empowers Casey to say whatever he wants whenever he wants to say it.”
One of the first lines Harrell chose to speak was to his toddler, Aya. “Sweet daughter of mine,” he said, “I have been waiting for this for a long time.”
The computer system enables Harrell to say some 125,000 words, which is more than twice the vocabulary of the average college graduate. And the system produces them with 97.5% accuracy — much higher than the 75% accuracy achieved in prior studies — a leap Brandman attributes in part to increasing the number of electrodes implanted.
“The outcomes have exceeded our expectations, says Brandman, who coauthored a 2024 paper on the effort. “This neuro-prosthesis began working the first day Casey tried it, and its accuracy exceeds that of any other communication device ever reported.”
What’s more, the system allows Harrell to speak with the sound of his own voice. To achieve that feature, the AI algorithms were trained on old recordings — podcast interviews Harrell conducted as a climate activist, for example — of his voice.
The algorithm has improved as Harrell has been using it, but it performed very well from the get-go, says Leigh Hochberg, MD, PhD, director of a consortium called BrainGate, which coordinates BCI work at several academic medical institutions, including UC Davis.
Hochberg describes an example from Harrell’s second day using the system. He recalls Harrell sharing that he was looking for a cheetah. “I assumed that had to be a decoding error, but it wasn’t, because Casey’s daughter had just walked in dressed as a cheetah.”
“The rest of the interaction after that was a close, personal, real-time conversation between a father and a daughter,” he says. “That’s the kind of impact that these technologies will have on the quality of people’s lives.”
The world’s first eye and face transplant

Aaron James receives the first full-eye and partial-face transplant in a surgery at NYU Langone Health that required the teamwork of some 140 health care professionals and lasted more than 20 hours.
Photo courtesy Joe Carrotta/NYU Langone staff
In June 2021, Aaron James’ life changed unimaginably. The Hot Springs, Arkansas, lineman was working on utility repairs when an exposed wire struck him, delivering a massive 7,200 volts to his face. The 46-year-old lost his nose, lips, chin, left eye, and part of his tongue.
Two years later, in a 21-hour surgery at NYU Langone in New York City, James became the world’s first recipient of a total-eye and partial-face transplant.
Today he is back home, leading a much fuller, healthier life. “I’m pretty much back to being a normal guy, doing normal things,” James said in a press release. “I’ve been given the gift of a second chance, and I don’t take a single moment for granted.”
The surgery — which required the expertise of more than 140 medical professionals — achieved several breakthroughs, as described in a 2024 JAMA Network article.
Among them is that the eye survived transplantation.
“The retina, blood flow, and eye pressure are healthy,” explains study senior author and NYU Langone reconstructive plastic surgeon Eduardo Rodriguez, MD, DDS. “The eye also retained its normal shape. Many experts believed it would shrink to the size of a raisin over time, but that hasn’t happened,” he says. “We couldn’t be happier with the results.”
As Rodriguez expected, the surgery didn’t restore sight in the eye, but he says the organ’s ongoing health marks great progress toward that goal for millions of other patients. NYU now joins a new, national effort focused on achieving vision-restoring whole-eye transplants.
James says he’s grateful to contribute to such efforts. “It feels so good to say, ‘Hey, I was part of that.’ It makes me stand up a little taller.”
Meanwhile, James says he’s benefited tremendously from his face transplant, as captured in a dramatic video.
“Before, Aaron relied on a feeding tube and a breathing tube. His face was terribly scarred, and his speech was unintelligible,” says Rodriguez. “Now he can eat whatever he wants, he can smell again, and he speaks normally. There has been a 180-degree improvement.”
What’s more, James has not had a single instance of transplant rejection, which is unusual. That’s partly because of a unique immunosuppression regimen, says Rodriguez, who had performed four previous face transplants.
Significant innovation and preparatory planning fueled the successful surgery.
For one, the team rehearsed logistics and techniques more than a dozen times before the actual transplant. They also used cutting-edge, patient-specific 3D guides to ensure the precise alignment of bones, plates, and screws. And they injected the donor’s adult stem cells into the eye to help improve nerve growth and prevent rejection.
“It’s been incredibly exhilarating,” says Rodriguez of the surgery. “It feels like we aimed to climb the Himalayas and succeeded.”
Still, he adds, much of the credit extends beyond the medical team.
“None of this is possible without the courage of people like Aaron,” he says. “And it wouldn’t be possible without the donor’s family, who were being brave and generous at one of the most difficult times of their lives.”
A no-needle treatment for severe allergic reactions

The first nasal spray to treat anaphylaxis could help save lives since many patients fear the shots that auto-injectors such as EpiPens require.
Courtesy ARS Pharmaceuticals
Millions of Americans live with allergies to commonplace triggers, from peanut butter to beestings.
That means they could be at risk for anaphylaxis, a severe reaction that can lead to difficulty breathing, vomiting, and dangerously low blood pressure. If not treated immediately, anaphylaxis can be fatal.
Yet huge numbers of allergic individuals fail to carry the standard anaphylaxis treatment: an EpiPen or other epinephrine auto-injector. In fact, fewer than half of patients at risk for severe allergic reactions carry the products with them regularly — and even those that do so often try to delay using them. Frequently, the cause is a fear of needles. Up to half of adolescents are afraid of shots, according to a meta-analysis, as are 20% to 30% of young adults.
Now, epinephrine can be delivered via a far less intimidating device: an epinephrine nasal spray called ARS-2, also known simply as “neffy.” The spray, approved earlier this year by the Food and Drug Administration (FDA), can be prescribed to patients as young as 4 as long as they weigh at least 33 pounds.
“Epinephrine saves lives, but it’s a major problem that people don’t use it, so this could be a big difference-maker,” says Jonathan Spergel, MD, PhD, chief of the Allergy Program at Children’s Hospital of Philadelphia.
Neffy offers other advantages over auto-injectors, says Spergel, who coauthored a 2024 Pharmaceutics paper evaluating the spray.
For one, the device is simpler to use. For example, children as young as 10 can successfully follow instructions for neffy, according to the manufacturer.
In addition, neffy is relatively small. Auto-injectors like EpiPens measure 6 inches tall, which makes carrying the recommended two doses a bit cumbersome. Neffy, on the other hand, is 2 inches high. It also has a longer shelf life, so it doesn’t require checking and replacing as often as the pens, he says.
Of course, such pluses aren’t significant unless the spray works as well as the shots.
Proving that was a bit complicated, says Spergel. “It wouldn’t be ethical to purposely make someone anaphylactic, so it’s not possible to do a head-to-head comparison,” he notes.
Instead, the FDA sought proof that the nasal spray succeeded with stand-in markers such as participants’ heart rates and the concentration of epinephrine in their bloodstream. Neffy achieved those measures. It did so even among patients with stuffy noses, says Spergel.
Another positive indicator is that in a small, real-world study, neffy worked among patients who developed anaphylaxis symptoms while being tested for food allergies. So although some doctors may suggest that any patient who previously had a severe allergic reaction carry an EpiPen as a backup, Spergel feels fine recommending neffy alone.
“This is very exciting,” he says. “It’s nice to know it can make things easier for people and even help save lives.”

